Introduction
Sciatica is a condition that has garnered considerable attention in both medical literature and popular discourse, affecting millions of individuals worldwide. Characterized by pain that radiates along the sciatic nerve— which runs from the lower back through the hips, buttocks, and down each leg—sciatica can significantly impair one’s quality of life. Understanding this condition is essential for those who experience it and healthcare professionals tasked with diagnosing and treating it. From an orthopedic perspective, sciatica is often a symptom of an underlying issue, such as a herniated disc, spinal stenosis, or degenerative disc disease. This article aims to delve into the complexities of sciatica, exploring its causes, risk factors, and treatment options while highlighting the importance of a holistic approach in managing this often debilitating condition. By enhancing our understanding of sciatica through an orthopedic lens, we can better equip ourselves to address its challenges and improve patient outcomes.
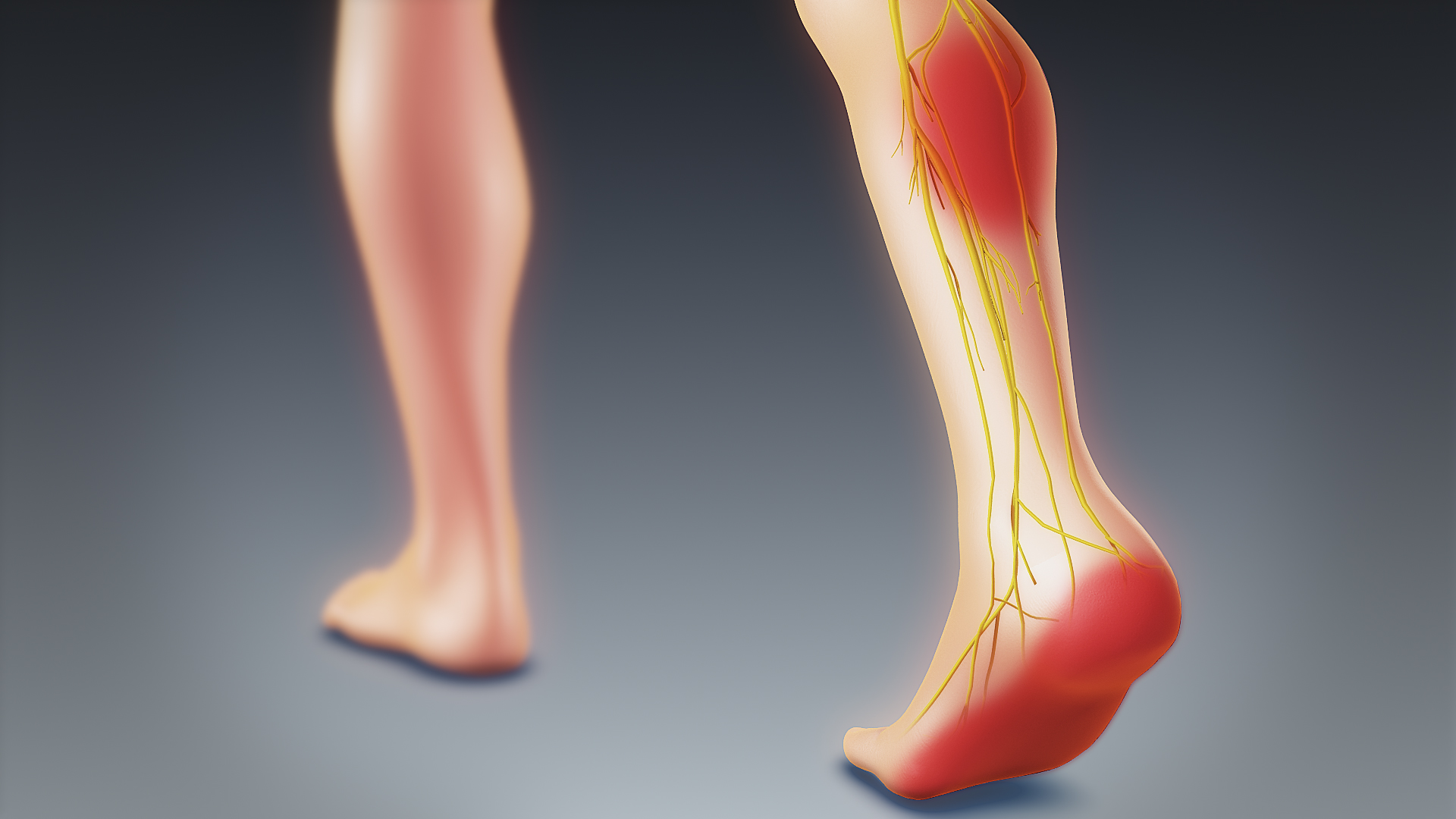
Anatomy of Sciatica
Sciatica is a term commonly used to describe the pain that radiates along the path of the sciatic nerve, which extends from the lower back down through the hips and buttocks and into each leg. Understanding the anatomy of sciatica is essential for effective diagnosis and treatment. This article will provide an overview of the sciatic nerve, related structures, and common anatomical issues that may lead to sciatica.
- Overview of the Sciatic Nerve
The sciatic nerve is the longest and thickest nerve in the human body, measuring about three-quarters of an inch in diameter. It originates from the lumbosacral plexus, which is formed by the spinal nerves L4 to S3. These nerve roots converge to form the sciatic nerve, which exits the pelvis through the greater sciatic foramen and passes beneath the piriformis muscle in the buttock region.
The sciatic nerve plays a crucial role in the sensory and motor function of the lower extremities. It innervates the muscles at the back of the thigh, including the hamstrings, and supplies sensation to the skin of the leg and foot, including the calf and the majority of the foot soles. The sciatic nerve then bifurcates into two main branches: the tibial nerve and the common peroneal nerve, which further descend into the lower leg and foot.
Given its long course, the sciatic nerve can be susceptible to various injuries and disorders that can manifest as pain, numbness, or weakness in the lower back, buttocks, and legs.
- Related Structures
Several anatomical structures are relevant to understanding sciatica, including:
a. Spinal Structures
The lumbar and sacral spine houses the nerve roots that contribute to the sciatic nerve. Intervertebral discs, which act as cushions between the vertebrae, can herniate or degenerate, leading to compression of the nerve roots.
b. Muscles
The piriformis muscle is particularly significant. It is located deep in the buttock and can irritate the sciatic nerve if it spasms or becomes tight, a condition commonly referred to as piriformis syndrome. Other muscles in the area, such as the gluteus maximus and hamstrings, can also impact the sciatic nerve.
c. Fascia and Ligaments
Fascia, a connective tissue that envelopes muscles and organs, and ligaments that stabilize the pelvis and spine can contribute to the entrapment or irritation of the sciatic nerve. Fascial restrictions or inflammation in the pelvic region can lead to altered dynamics that may compress the sciatic nerve.
d. Blood Vessels
The sciatic nerve runs closely with the blood vessels in the region, such as the inferior gluteal artery, which can impart pressure on the nerve or be affected by vascular disorders.
- Common Anatomical Issues
Several conditions can lead to sciatica, typically resulting from anatomical factors that can compress or irritate the sciatic nerve:
a. Herniated Discs
When a spinal disc herniates, the inner gel-like material can protrude through the outer layer and compress the nearby nerve roots. This is one of the most common causes of sciatica, especially in middle-aged adults.
b. Spinal Stenosis
Spinal stenosis refers to the narrowing of the spinal canal, which can put pressure on the sciatic nerve roots. This condition is often related to age, degenerative disc disease, or arthritis, leading to pain that worsens with movement.
c. Degenerative Disc Disease
As discs age and lose hydration and elasticity, they may become flattened and less effective at cushioning spinal vertebrae, contributing to pressure on the nerves.
d. Piriformis Syndrome
As previously mentioned, tightness or spasms in the piriformis muscle can compress the sciatic nerve, leading to pain that can mimic sciatica but is due to muscle issues rather than spinal problems.
e. Spondylolisthesis
In this condition, one vertebra slips forward over another, potentially pinching the sciatic nerve roots and causing pain along the nerve’s pathway.
f. Trauma or Injury
Injuries to the lower back or pelvis can also lead to sciatica, whether through direct trauma, fractures, or inflammation that results in sciatic nerve compression.
Understanding the anatomy of sciatica, including the structure and function of the sciatic nerve and associated anatomical components, is vital for diagnosing and treating sciatica effectively. Conditions such as herniated discs, spinal stenosis, and piriformis syndrome can lead to sciatica symptoms, emphasizing the importance of early intervention and tailored therapeutic approaches. Armed with this knowledge, patients and healthcare providers can work together to alleviate the pain and dysfunction that often accompany this common condition.
Understanding the Causes of Sciatica
Sciatica is a term used to describe symptoms of pain, tingling, or numbness that radiate along the path of the sciatic nerve, which branches from the lower back through the hips and buttocks and down each leg. While sciatica is often associated with lower back issues, it can stem from various underlying causes. Understanding these causes and associated risk factors is crucial for effective management and prevention.
- Common Causes of Sciatica
Herniated Discs
One of the most prevalent causes of sciatica is a herniated disc, also known as a slipped or ruptured disc. The spine is made up of intervertebral discs that act as cushions between the vertebrae. When a disc herniates, its outer layer tears, allowing the soft inner material to protrude and press against nearby nerves, including the sciatic nerve. This compression can lead to pain that radiates along the nerve pathway.
Degenerative Disc Disease
Degenerative disc disease is another common cause of sciatica, particularly in older adults. As we age, the intervertebral discs lose hydration and elasticity, leading to a decrease in height and disc integrity. This degeneration can lead to spinal instability and osteophyte (bone spur) formation, which may impinge on the sciatic nerve.
- Less Common Causes of Sciatica
Spondylolisthesis
Spondylolisthesis occurs when one vertebra slips forward over another, which can compress or irritate the sciatic nerve. This condition may be congenital or the result of wear and tear over the years. Although less common, it can lead to significant discomfort and impair functional mobility.
Tumors
While rare, tumors within the spine or surrounding tissues can press against the sciatic nerve, resulting in sciatic nerve pain. These tumors can be benign or malignant and may require medical evaluation to determine appropriate treatment options.
Infections
Infections related to the spine, such as spinal osteomyelitis or discitis, can also lead to sciatica. If infected discs or vertebrae impinge on nerve roots, it can cause severe pain and other neurological symptoms that mirror sciatica. Prompt medical attention is essential for addressing infections to prevent further complications.
- Risk Factors for Sciatica
Recognizing the risk factors for developing sciatica can help in prevention and early intervention. Here are some of the key risk factors:
Age
The likelihood of experiencing sciatica increases with age, particularly as the spinal discs degenerate over time. Conditions like herniated discs and degenerative disc disease become more common among older adults, making sciatica a frequent complaint in this population.
Obesity
Excess body weight can increase stress on the spine, leading to conditions that trigger sciatica. Obesity is associated with inflammation and disc degeneration, enhancing the risk of nerve compression and resultant pain.
Sedentary Lifestyle
A lack of physical activity contributes to weakening core and back muscles, which are vital for supporting the spine. Sedentary behavior can also lead to poor posture, further increasing the likelihood of conditions that cause sciatica.
Occupational Hazards
Jobs that require heavy lifting, long periods of sitting, or repetitive movements can place strain on the back and lower spine. These occupational hazards can lead to an increased risk of developing conditions that result in sciatica.
Sciatica can significantly impact an individual’s quality of life, making it essential to understand its causes, risk factors, and symptoms. While common conditions like herniated discs and degenerative disc disease are frequent culprits, less common causes, such as tumors and infections, also warrant consideration. By being aware of risk factors like age, obesity, a sedentary lifestyle, and occupational hazards, individuals can take proactive measures to mitigate their risk and seek timely treatment. If you experience symptoms of sciatica, consult a healthcare professional for a comprehensive evaluation and personalized management plan.
Symptoms and Diagnosis of Sciatica
Sciatica is a term that refers to a set of symptoms resulting from the irritation of the sciatic nerve, which originates in the lower back and travels through the buttocks and down the legs. Understanding the symptoms and diagnostic approaches is crucial for effective treatment and management of this condition. This article will explore the primary symptoms of sciatica, the diagnostic techniques employed by medical professionals, and the conditions that may mimic this common ailment.
- Recognizing Sciatica Symptoms: Pain, Numbness, and Tingling Patterns
The hallmark symptom of sciatica is pain that radiates from the lower back down through the buttock and into the leg, following the path of the sciatic nerve. This pain can vary in intensity and may be described as sharp, burning, or stabbing. It may also feel like a persistent ache.
Common Symptoms Include:
Lower Back Pain: This pain is often localized in the lower back and can range from mild discomfort to intense pain.
Radiating Pain: Pain may spread down one leg, often reaching the knee or even the foot. Patients may experience shooting pains that make it difficult to sit, stand, or walk.
Numbness and Tingling: Some individuals may notice numbness, tingling, or a “pins and needles” sensation that follows the sciatic nerve pathway. This sensation can indicate nerve involvement and may affect the calf or foot.
Muscle Weakness: In some cases, there may be a noticeable weakness in the affected leg, leading to difficulty with mobility or performing certain physical activities.
Recognizing these patterns of symptoms is crucial for patients who may be experiencing sciatica, as they may help prompt a visit to a healthcare professional for further evaluation.
- Diagnostic Technique: Physical Examination and Imaging Techniques
Upon reporting symptoms consistent with sciatica, a healthcare provider typically begins with a thorough physical examination. During this examination, the doctor may assess:
Range of motion: How well the patient can move their back and legs.
Strength: Evaluating muscle strength in the affected leg.
Reflexes: Checking reflex responses in the legs to identify nerve involvement.
Imaging Techniques:
If sciatica is suspected, or if symptoms are severe or persist, doctors may order imaging studies to determine the underlying cause of nerve compression. Common imaging techniques include:
MRI (Magnetic Resonance Imaging): This non-invasive technique provides detailed images of soft tissues, including disks, nerves, and spinal cord structures. An MRI can reveal herniated or bulging disks that may be pressing on the sciatic nerve.
CT Scans (Computed Tomography): This imaging method is useful for a comprehensive view of the spine and can help visualize bone structures, disk abnormalities, and other potential causes of nerve compression.
Both MRI and CT scans offer invaluable insights and aid significantly in developing an effective treatment plan by identifying the root cause of sciatic nerve irritation.
- Differential Diagnosis: Conditions that Mimic Sciatica
While sciatica is a common condition, several other medical issues can produce similar symptoms, leading to a potential misdiagnosis. Differential diagnosis is essential in ensuring that patients receive appropriate treatment. Conditions that may mimic sciatica symptoms include:
Piriformis Syndrome: In this condition, the piriformis muscle, located in the buttock region, can spasm and irritate the sciatic nerve, leading to symptoms that closely resemble those of sciatica. Pain from piriformis syndrome may also be exacerbated by prolonged sitting or specific activities.
Herniated Disks: While herniated disks are often a cause of sciatica, they can also present independently with similar pain patterns without nerve involvement.
Spinal Stenosis: This narrowing of the spinal canal can compress the spinal cord and nerves, leading to pain and nerve-related symptoms.
Sacroiliac Joint Dysfunction: Dysfunction in the sacroiliac joint can lead to referred pain similar to sciatica, primarily affecting the lower back and buttocks.
Lumbar Radiculopathy: This condition involves damage or irritation of the lumbar nerve roots, which can produce similar symptoms, making it essential to rule it out during diagnosis.
By carefully differentiating sciatica from these related conditions, healthcare providers can ensure patients receive the most effective treatment tailored to their specific diagnosis.
Sciatica can significantly affect quality of life, with its characteristic pain, numbness, and tingling disrupting daily activities. Proper diagnosis is essential for effective management, relying on a thorough physical examination and appropriate imaging techniques. Additionally, awareness of conditions that may mimic sciatica is vital for accurate diagnosis and treatment. Seeking professional help at the early signs of sciatica can lead to timely interventions, lessening the chance of chronic issues and improving overall outcomes.
Conclusion and Future Directions in Sciatica Research and Care
Sciatica, characterized by pain radiating along the pathway of the sciatic nerve, remains a prevalent issue affecting a significant portion of the population. Currently, it represents a challenging condition due to its multifaceted nature involving various etiologies and patient responses to treatment. As the landscape of research evolves, emerging therapies and studies provide promising solutions. Furthermore, the role of orthopedic specialists in managing sciatica exemplifies the critical nexus between advanced medical knowledge and enhanced patient care. To achieve the best possible outcomes, it is essential for patients to take proactive steps by seeking early intervention and consulting orthopedic experts.
Current Trends in Research: Emerging Therapies and Studies on Sciatica
Recent research has unveiled a variety of innovative therapies designed to alleviate sciatica symptoms and address underlying causes. Among these, minimally invasive surgical options, regenerative medicine approaches such as platelet-rich plasma (PRP) injections, and the integration of physical therapy and conservative management are showing promise. Notably, regenerative therapies focus on healing tissues and nerves rather than merely masking pain, offering a more holistic approach to treatment.
Evaluating the effectiveness of these emerging therapies is a vital area of current research. Studies are exploring the long-term benefits and risks associated with different modalities of treatment, from pharmacological interventions to surgical corrections. Furthermore, ongoing investigations are enhancing our understanding of the biological mechanisms underlying sciatica, paving the way for precision medicine tailored to individual patient profiles.
As the field continues to flourish, interdisciplinary collaborations between orthopedic specialists, pain management experts, and rehabilitation professionals will yield more comprehensive treatment protocols. Future research endeavors should prioritize both the efficacy and safety of emerging therapies, ensuring that patients benefit from the most contemporary, evidence-based practices.
The Role of Orthopedic Specialists: Enhancing Patient Care
Orthopedic specialists play an indispensable role in the management of sciatica. Their extensive training in musculoskeletal disorders equips them with the expertise to accurately diagnose the root cause of sciatica, which may stem from herniated discs, spinal stenosis, or other conditions affecting the lumbar region.
Through comprehensive assessments — including imaging studies and physical exams — orthopedic specialists can devise tailored treatment plans that may involve minimally invasive surgery, physical rehabilitation, or targeted injections. Their deep understanding of biomechanics and anatomy allows for precise interventions that optimize recovery and minimize complications.
Moreover, orthopedic specialists are instrumental in guiding patients through the continuum of care, ensuring they are informed and actively engaged in their treatment journey. Education on lifestyle modifications, exercise regimens, and ergonomic adjustments can empower patients, fostering an environment of healing and prevention.
Seek Early Intervention and Orthopedic Consultation
Given the varied presentations and potential complications associated with sciatica, seeking early intervention is paramount. Delaying treatment can lead to worsening symptoms, chronic pain, and decreased quality of life. Patients experiencing symptoms of sciatica, including pain, tingling, or weakness in the lower back and legs, are encouraged to take proactive measures.
Consulting with DR. AMIT ROY, best orthpedic surgeon in kolkata & burdwan. Visit- www.dramitroy.com/my-clinics
In conclusion, the future of sciatica management looks promising, with emerging therapies and comprehensive orthopedic care leading the charge toward more effective and personalized treatment. Patients are encouraged to break the cycle of chronic pain by seeking early intervention and the expertise of orthopedic specialists — an investment in their health and well-being that can yield lifelong benefits.